Dialectical Behavior Therapy (DBT) for Addiction Treatment in East Texas
Addiction is a complex and multifaceted condition, often intertwined with mental health disorders, trauma histories, and difficulties managing emotions. It can often intersect with emotions, trauma, and distressing topics from one’s past that may influence a person’s ability to cope in the present.
For many individuals, traditional individual therapy alone isn’t enough to break free from substance dependence. At Cypress Lake Recovery, we incorporate evidence-based therapeutic approaches like Dialectical Behavior Therapy (DBT) to address both addiction and its underlying emotional drivers.

What is Dialectical Behavior Therapy (DBT)?
Dialectical Behavior Therapy, commonly known as DBT, is a type of cognitive-behavioral therapy (CBT) developed by psychologist Dr. Marsha Linehan in the late 1980s. Originally designed to treat borderline personality disorder, DBT has since been adapted and proven effective for a range of mental health conditions as well as addiction.
Unlike standard CBT, which focuses mainly on thought patterns, DBT combines cognitive techniques with concepts of mindfulness, acceptance, and distress tolerance. The therapy is “dialectical” because it integrates two opposing ideas: acceptance of current experiences and commitment to change. This balance allows clients to feel validated while also being encouraged to make healthier decisions.
DBT typically involves four main modules:
- Mindfulness: Developing awareness of the present moment without judgment. This skill teaches clients to observe their thoughts, feelings, and bodily sensations with curiosity rather than criticism, helping reduce impulsive behaviors driven by uncomfortable emotions.
- Distress Tolerance: Learning how to tolerate pain or crisis situations without resorting to substance use or other self-destructive coping mechanisms. Techniques might include distraction, self-soothing practices, and radical acceptance of what cannot be immediately changed.
- Emotion Regulation: Understanding and managing intense emotions that often lead to substance use or relapse. Clients learn to identify emotional triggers, reduce emotional vulnerability through self-care, and increase positive emotional experiences.
- Interpersonal Effectiveness: Strengthening communication skills to assert needs, set boundaries, and maintain healthy relationships without aggression or withdrawal.
For individuals battling addiction, DBT provides a structured framework to build emotional resilience and practical tools for sobriety.
The Goals of DBT
The primary goals of DBT in addiction treatment revolve around enhancing a person’s quality of life by equipping them with strategies to manage emotions and behaviors that interfere with recovery. The exact plan for recovery and accompanying goals may look different for every individual, depending on their treatment plan.
Key goals may include:
- Reducing Life-Threatening Behaviors: For those struggling with severe addiction, overdose and related risks are life-threatening. DBT prioritizes reducing these behaviors first to keep clients safe.
- Eliminating Therapy-Interfering Behaviors: These include missing sessions, emotionally shutting down during therapy, or failing to complete recovery assignments. DBT encourages accountability and therapeutic engagement.
- Decreasing Quality-of-Life-Interfering Behaviors: This covers behaviors such as substance use, self-harm, or sabotaging relationships that impact overall well-being.
- Enhancing Skills for a Life Worth Living: Perhaps the most meaningful goal, DBT helps clients create and pursue a vision for their lives beyond addiction. This includes building purpose, healthy relationships, and emotional stability.
Contact Our Admissions Team Today
Benefits of DBT for Addiction
DBT is a powerful tool within addiction treatment because it addresses the emotional dysregulation at the heart of many substance use disorders. Core benefits of incorporating DBT may include:
One of the most challenging aspects of recovery is finding healthy alternatives to drugs or alcohol for managing stress, anxiety disorders, and emotional pain. DBT teaches practical coping mechanisms, including grounding exercises, mindfulness practices, and distress tolerance techniques. Clients learn to sit with discomfort without reacting impulsively, helping prevent relapse during triggering situations. This shift helps the person build confidence in their ability to navigate daily life without substances.
Many people use substances to escape overwhelming feelings or crisis moments. DBT equips clients with distress tolerance skills, such as:
- Self-Soothing: Using senses (touch, taste, smell, sound, sight) to calm the nervous system.
- Distraction: Redirecting attention to neutral or positive activities until distress passes.
- Radical Acceptance: Embracing reality as it is (even if painful) rather than fighting it.
- Pros and Cons Analysis: Evaluating the consequences of using versus coping in healthier ways.
These tools can empower clients to move through urges and cravings without giving in to them.
A large proportion of individuals with addiction also struggle with mental health disorders, such as depression disorders, anxiety, post-traumatic stress disorders (PTSD), or personality disorders. DBT can be particularly effective for dual diagnosis because it:
- Addresses Emotional Dysregulation: Many mental health conditions involve difficulty managing emotions, which can drive addictive behaviors. DBT directly targets these patterns.
- Provides Structure: The skills-based approach gives clients clear strategies to manage both mental health symptoms and addiction triggers.
- Promotes Mindfulness: This aspect is beneficial for managing symptoms of depression, anxiety, and trauma, which in turn reduces the desire to self-medicate.
Another critical benefit of DBT is its focus on building a life worth living. Recovery is not only about avoiding substances but about creating a meaningful, fulfilling life that feels aligned with personal values. DBT helps individuals identify what matters most to them and take actionable steps towards those goals.
For example, individuals may set goals around repairing relationships, pursuing education, exploring spirituality, or volunteering during times when they might otherwise be using drugs. These goals can provide motivation to remain sober while also fostering purpose and self-worth.

Testimonials
![]()
![]()
![]()
![]()
![]()
Regina
I am so happy that I chose Cypress to begin my recovery. I have suffered for years from depression, anxiety, panic disorder, and PTSD. The programs that are offered here at Cypress have been truly phenomenal in helping me recover. I also appreciated the professional staff that are here on duty 24/7, which helps create a safe environment. Cypress Lake Recovery uses effective “one on one” methods that meet each person’s individual needs because they evaluate and have a better understanding of your personal traumatic experiences. Thanks Sabino, I am truly grateful to you and the Cypress family.
![]()
![]()
![]()
![]()
![]()
J.A.
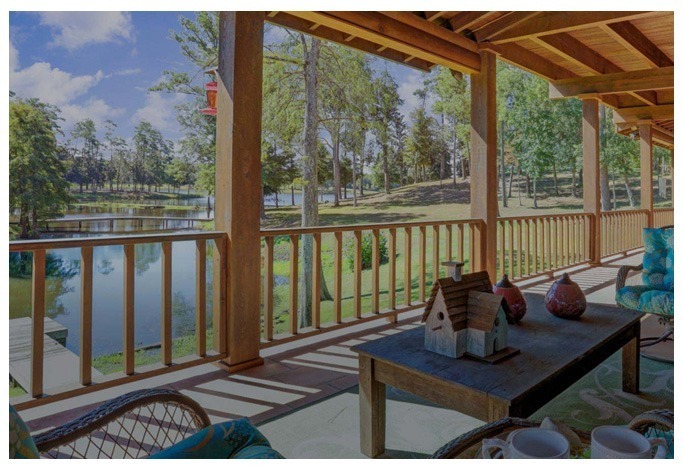
A beautiful facility! Staff sets the tone and kindness that residents easily follow. Thank you, Cypress Lake Recovery!
![]()
![]()
![]()
![]()
![]()
Pamela
The program at Cypress Lake Recovery works! I emerged from an accumulation of unrecognized emotions, issues of trust, and unresolved grief and loss. 35-days of effective integration of customized quality therapy reconnected my mind, body, spirit, and I am worth it! I had masked emotions and hurtful events for decades with alcohol. At Cypress Lake Recovery I safely focused deep within to unleash harmful secrets and self-degradation. Tools of recovery were practiced, not just presented. Integrative therapies were tailored to my circumstances, thus were effective. This residential program is like no other. For me, Cypress Lake Recovery delivered what was professed. I am forever grateful for this gift of healing.
![]()
![]()
![]()
![]()
![]()
Mike
Life changing experience. Wonderful staff. Wonderful program. Thanks for everything!
![]()
![]()
![]()
![]()
![]()
Darcy
It was great to begin my recovery in a group environment with so many knowledgeable nurses, therapists, BHT’s, and others around for support. The equine therapy, challenge course, family week, and daily therapies all work together seamlessly, allowing me to leave Sabino as a healthier and stronger person!
The Importance of Dual Diagnosis Treatment for Addiction
How Mental Illness and Addiction Interact
- Self-Medication: Individuals with depression, anxiety, or PTSD may turn to substances to numb emotional pain, reduce anxiety, or feel temporary relief.
- Aggravated Mental Health: Substance abuse can exacerbate symptoms of mental illness, leading to a vicious cycle where mental health worsens, prompting more substance use.
- Shared Risk Factors: Genetics, trauma history, and environmental stressors often underlie both mental illness and addiction.
For example, a person with borderline personality disorder may struggle with intense emotional pain and fear of abandonment. Without treatment, they may use alcohol or drugs to cope with these feelings, only to find that substance use worsens their relationships and emotional stability.
The Need for Integrated Treatment
- Teaching emotional regulation skills that help with regulating mental health symptoms and lessening the need for self-medication.
- Building distress tolerance, which reduces reliance on substances during emotional crises.
- Providing practical tools for navigating interpersonal challenges that may otherwise trigger relapse.
For instance, if a client with PTSD learns distress tolerance and emotion regulation through DBT, they may be better equipped to manage trauma-related triggers without turning to drugs or alcohol. This integrated approach results in more durable, stable recovery outcomes.
Heal From Addiction at Cypress Lake Recovery
We recognize that recovery is not just about abstaining from substances but about building a life you no longer feel the need to escape from. Through DBT, individuals can develop:
- Mindful Awareness: Cultivating presence to manage cravings and triggers.
- Emotional Resilience: Learning to handle distress without self-destructive behavior.
- Improved Relationships: Building healthy communication and setting boundaries.
- Personal Empowerment: Developing confidence to make choices aligned with long-term goals.
We understand that no two recovery journeys are the same, and we honor each person’s path by providing personalized care that supports the mind, body, and spirit.
Start Your Healing Journey Today
Nationally Recognized & Accredited





- Linehan, M.M. (1993). Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford Press.
- Linehan, M.M., et al. (1999). Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. American Journal on Addictions, 8(4), 279-292. https://pmc.ncbi.nlm.nih.gov/articles/PMC2797106/
- National Alliance on Mental Illness. Dual Diagnosis.



